Macular Degeneration
Macular degeneration: This is a common condition, often asymptomatic, which affects older individuals increasingly after the age of 60. Less commonly it can affect younger people, especially if they are very nearsighted. The macula is the center of the retina in the back of the eye and is responsible for the central part of the vision allowing us to read and see fine detail. With age, this central portion of the retina can undergo degenerative changes which, if severe, can lead to serious loss of central vision. Recently it has become clear that genetics plays a major role in the susceptibility to macular degeneration and a family history of it in parents and siblings is a risk factor. Other risk factors include smoking, female gender, light-colored eyes, and farsightedness.
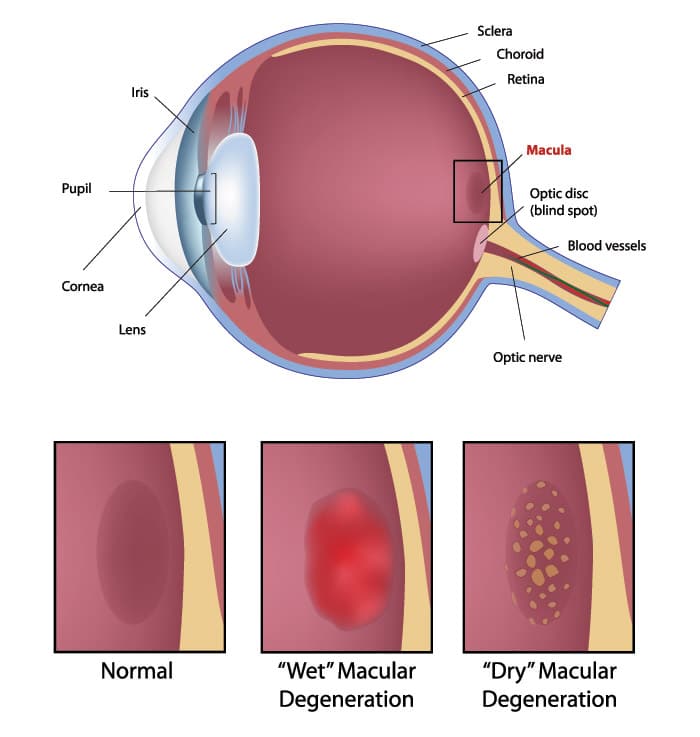
Macular degeneration is usually divided into two categories: wet and dry. The dry form is more common and usually has much less effect on the vision. In this case, the pigment layer behind the macula undergoes atrophy and can accumulate deposits of waste material, called “drusen”, which are visible to the ophthalmologist as yellowish spots in the back of the eye. Many times, dry macular degeneration may not affect the vision, but in more severe cases the vision can become blurred or blind spots or blank areas may appear in the central vision. There is no known effective way of improving dry macular degeneration, but it has been proven that the antioxidant vitamins A, E, C, and Zinc, in specific doses, can slow its progress and reduce the risk of vision loss. These should only be taken after consultation with a medical doctor as they can have side effects.
Wet macular degeneration is so-called because it is the result of tiny abnormal new blood vessels that grow and break into the space behind the macula, causing leakage of blood and fluid. It is often preceded by dry degeneration, and an exam by an ophthalmologist can identify people who may be asymptomatic but at risk for the development of this more severe form of the disease. Wet macular degeneration is less common, but when it occurs can cause more serious loss of vision. Symptoms may begin as gradual progressive blurring or distortion of the vision. Straight objects such as telephone poles or Venetian blinds may appear crooked. Sometimes the loss of vision occurs abruptly and with no warning. People with this form of the disease in both eyes who are either not treated, or who do not respond well to treatment, may end up losing the ability to read, drive or recognize faces, but almost never lose their peripheral vision. They, therefore, remain able to function independently although they may require assistance in tasks involving reading and transportation.
Macular degeneration can be diagnosed by an ophthalmologist with a dilated fundus exam in the office. Many times another in-office testing, such as angiography, a photographic test involving an injection of intravenous dye, or ocular coherence tomography, a sophisticated digital imaging test of the macula, may be necessary to diagnose and formulate the appropriate treatment, if any, for the problem.
Over the last few years, several treatments for wet macular degeneration have become available which can halt its progression and, in some cases, even reverse the loss of vision. These commonly include medications, such as Lucentis, Avastin or Triamcinolone, which are injected directly into the eye in a procedure called an intravitreal injection. This is a quick procedure that is performed in the office and has few side effects. Many patients initially find the idea of these injections quite disturbing, which is a natural reaction. The reality, however, is that the procedure is usually very well tolerated and most patients who undergo it are surprised and relieved at how relatively painless and easy it is. Photodynamic therapy is another treatment that is sometimes employed in the office, involving an injection of a medication called Visudyne into a vein of the arm. Fifteen minutes after the start of the injection, a low power red light laser is used to activate the medication in the back of the eye in order to seal off the leaking blood vessels under the macula. This procedure is often combined with an intravitreal injection. Patients must completely avoid sun exposure for up to five days after the procedure or severe sunburn may occur. Conventional hot laser treatment may still sometimes be employed to cauterize the leaking vessels but this treatment is less commonly performed now than in years past when it was the only treatment available. Unfortunately, none of these treatments are effective in all patients, and even when effective often need to be repeated periodically to control the disease. Macular degeneration is a chronic disease that can be treated but, as of today, has no cure. There is much ongoing research on macular degeneration and many experimental treatments are being tested in academic centers. Some of these will certainly lead to further improvements in treatment in the future. Unfortunately, there are also many completely unproven and, in fact, fraudulent treatments being promoted, often at high expense, through the internet and elsewhere. Patients are strongly advised to seek the opinion of an ophthalmologist prior to embarking on any of these “new” expensive therapies.

