Diabetic Eye Exams
The most common endocrine disorder in the world is Diabetes Mellitus. Its rate is increasing as obesity increases among the people in industrialized countries. It is caused by abnormalities in the ability of the body to metabolize circulating blood glucose (sugar) into stored carbohydrates and fats. This causes elevations in levels of circulating blood glucose. In some way, the small blood vessels in the body are damaged by this elevation causing harm to the kidneys, heart, brain, feet and the eyes. Type 1 Diabetes is seen in young patients but represents only 10% of all diabetics. It is often referred to as Juvenile Diabetes. The insulin-producing cells in the pancreas are destroyed. Type 2 Diabetes is seen in older patients and referred to as Adult Onset Diabetes. Type 2 diabetics have circulating insulin but show resistance at the receptor levels of metabolism so that blood glucose remains elevated.
How can my diabetes affect my eyes?
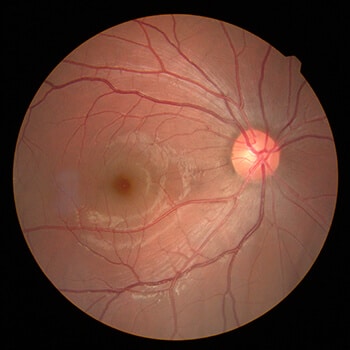
Diabetes may affect the eye in many ways including problems with focusing, trouble with moving the eyes causing double vision, drooping of the eyelids, early cataract formation and swelling of the retina. By examining the blood vessels in the retina in the back of the eye, the physician can often see any signs of damage typically caused by diabetes. This is the reason all diabetics must have a yearly evaluation of their eyes in order to help protect and treat them.
The better the control of diabetes by the patient, the less there is a chance for damage that can lead to bleeding, scarring, retinal detachment and other complications of diabetes called Diabetic Retinopathy. During the first two decades of disease, nearly all patients with Type 1 Diabetes and 60% of patients with Type 2 Diabetes will have Diabetic Retinopathy. Diabetes can even damage the eye so severely that it causes blindness. Diabetic Retinopathy is the most frequent cause of new cases of blindness among adults aged 20 –74 years.
Treatment Options
Treatment for the damaging effects of Diabetic Retinopathy includes laser photocoagulation, medications given in the eye to reduce vision treating retinal swelling and surgical repair of retinal detachment. Research continues to give us new tools for the diagnosis and treatment of diabetic patients.

