Crosslinking for Keratoconus
Keratoconus is a progressive eye condition where the cornea (the clear, dome-shaped front surface of the eye) starts to change shape. The cornea becomes steeper and slowly becomes thinner, eventually progressing into a cone shape. This irregular shape causes blurred vision and can lead to significant vision loss if not treated.
Keratoconus is considered a genetic condition, although there is not a single gene but rather a set of genes that increase the risk for keratoconus. Eye rubbing is also a known risk factor for keratoconus.
The goal for keratoconus is to identify patients early, before significant vision loss has occurred. Some of the common symptoms of keratoconus include blurred vision, changes in a patient’s glasses or contact lens powers, increasing astigmatism, or ghosting. Ghosting is a common visual phenomenon often experienced by individuals with moderate to severe keratoconus. It refers to seeing multiple images or “ghost” images around a single object. This can occur in one or both eyes and is particularly noticeable when looking at lights or high-contrast objects.

Can Keratoconus Develop Following Eye Surgery?
Keratoconus can develop after any eye surgery, although statistically eye surgery is not a common risk factor for keratoconus. At our center, we have cared for patients who have developed keratoconus many years after LASIK, PRK, Radial keratometry and corneal transplants. The history of these surgeries in most cases does not appear to be a risk factor for developing keratoconus. However, when patients have a history of corneal procedures, the condition can also be named post-LASIK ectasia, post-PRK ectasia, Post-RK ectasia, and post-corneal transplant ectasia. The vast majority of our patients with keratoconus have not history of any eye surgery
Crosslinking Overview
There are a variety of treatments available for patients with keratoconus. Crosslinking is considered the first line treatment, and should be considered when the condition has been diagnosed. The goals of crosslinking are to stop the progression of keratoconus. Most patients experience improvement in their corneal shape over 1 year to many years. The risk for needing a second crosslinking procedure is approximately 1%, meaning that 99% of patients only require 1 CXL procedure. It is of course important to stop eye rubbing, as eye rubbing is a known risk factor for requiring a second CXL procedure.
Thin Corneas With Keratoconus
With more advanced keratoconus, the cornea can become quite thin. The good news is that studies as well as our Center’s experience have found that patients with very thin corneas can safely undergo CXL with a very low risk of complications. In extremely thin corneas- under 200 microns – our centers have techniques for CXL that allow for the procedure to be performed safely with low risk. The goal for patients with very thin corneas is to prevent further progression of keratoconus that can potentially lead to the need for a corneal transplant.
Of note – when patients have very very thin corneas, they are at risk for a condition called hydrops, which can occur with or without having undergone CXL. Crosslinking does not increase or decrease the risk for developing hydrops in advanced keratoconus.
Patients Over the Age of 40 With Keratoconus
There is a misconception that patients over the age of 40 do not progress. We presented data from our Center that found 41% of patients between the age of 40 and 81 had progressive keratoconus. Progression of keratoconus is not linear. Patients can be relatively stable for many years, and then progress. Crosslinking strengthens the cornea, and prevents progression in approximately 99% of patients at our center.
Crosslinking Procedure
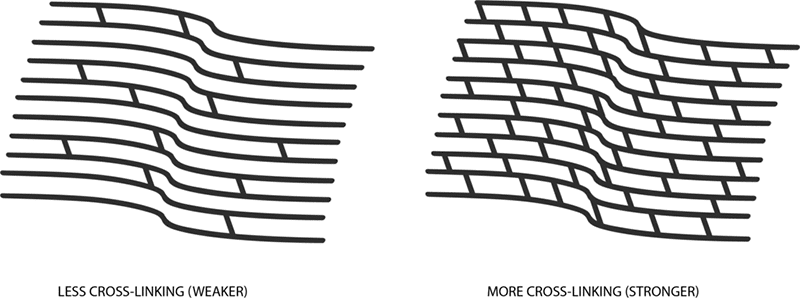
Corneal crosslinking (CXL) is a minimally invasive procedure designed to strengthen the cornea by increasing the number of natural crosslinks in the collagen fibers within the cornea. This helps to halt the progression of keratoconus. Riboflavin drops are placed on the cornea for approximately 30 to 40 minutes. Then, the cornea is examined to ensure saturation of the cornea with riboflavin. Then, Glaukos KXL light is used to treat the cornea for 30 minutes. This interaction between the riboflavin and UV light strengthens the collagen fibers in the cornea.
The procedure is painless. We recommend that patients have a driver to take them home followin the procedure. Patients will be given lubricating drops and anesthetic drops, which are used for the first 8 to 12 hours to help with eye discomfort.
Types of Crosslinking
Epithelium-Off (epi-off) Crosslinking
Epithelium-Off (epi-off) Crosslinking: The epithelium is removed before applying riboflavin. This method has insurance coverage. Center for Excellence In Eye Care was part of the initial FDA clinical trial in 2008 that led to the approval of Epithelial off CXL in 2016. Some commercial insurances provide coverage for Epithelial-off CXL
Epithelium-On (epi-on) Crosslinking
Epithelium-On (epi-on) Crosslinking: The epithelium is left intact. This method is less invasive and allows for less risk and faster visual recovery. William Trattler, MD was one of the first ophthalmologists in the US to perform Epi-On CXL in March 2010. The Center for Excellence In Eye Care has been part of 4 Epi-On Clinical trials starting in 201, and has therefore been able to treat patients with this technique for more than 14 years. Our Center is currently in the EpiOn FDA clinical trial, and has extensive experience with this technology.
Benefits of Crosslinking
- Halts the progression of Keratoconus
- May improve corneal shape and vision, over many months and years, in approximately 85% of cases
- Dramatically reduces the need for corneal transplants
Risks and Side Effects
- Temporary discomfort or pain
- Eye redness and irritation
- Hazy vision or light sensitivity during the initial healing period
- Rarely, infection or other complications (extremely rare with Epi-On)
Recovery and Aftercare
- Immediate Aftercare: Use prescribed antibiotic and anti-inflammatory eye drops
- Healing Period: Vision may be blurry for a few days and occasional 1-3 weeks. Many patients can return to normal activities within a day to a few days.
- Follow-Up: Regular follow-up visits with your eye doctor to monitor the healing process and the effectiveness of the treatment.
Consultation with an Eye Specialist It is important to have a thorough evaluation and discussion with an eye specialist to determine if crosslinking is the right treatment for your specific condition. Corneal crosslinking is an effective treatment for keratoconus that can halt the progression of the disease and preserve vision. Understanding the procedure, its benefits, and potential risks can help patients make informed decisions about their eye health.

